Karen Martin, MPH,1Rajal Mody, MD, MPH,1,2Malini Desilva, MD, MPH,1Emily Banerjee, MPH,1Anna Strain, PhD,1Stacy Holzbauer, DVM, MPH, DACVPM,1,2Cynthia Kenyon, MPH,1Melissa McMahon, MPH,1Paul Rota, PhD,3Paul Gastanaduy, MD, MPH,3Miriam Muscoplat, MPH,1Victoria Hall, DVM MS,1,4 and Kristen Ehresmann, MS, RN1Author informationCopyright and License informationDisclaimer
Abstract
Background
During April–June 2017, Minnesota experienced the state’s largest measles outbreak in 27 years. A vaccination campaign was implemented. Numerous vaccine-associated rash illnesses (VARI) were detected. VARI is non-contagious, but difficult to distinguish from measles clinically. Often, public health control measures need to be implemented before wild-type measles can be differentiated from VARI by viral genotyping. We compared clinical characteristics of VARI and confirmed measles cases to inform testing practices.
Methods
We defined measles cases per the Council of State and Territorial Epidemiologists. VARI was defined as a rash occurring in a person within 21 days after receipt of measles, mumps, and rubella (MMR) vaccine, and in whom a measles vaccine strain (genotype A) was detected in naso/oro- pharyngeal swab or urine samples. Minnesota’s immunization information system monitored MMR doses administered. We collected clinical information through routine case investigation.
Results
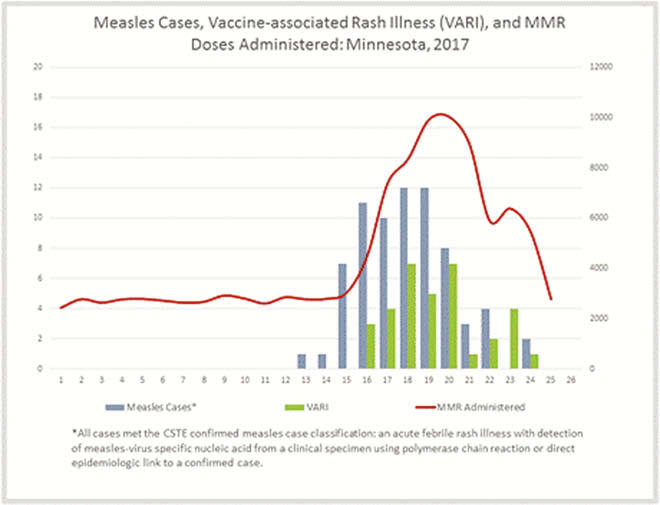
Over 42,000 MMR doses above expected were administered during the outbreak. We identified 71 measles cases and 30 VARI. The median age of VARI patients was 1.2 years (range 10 months–48 years) and for measles cases 2.8 years (range 3 months–57 years). VARI diagnosis increased with rising MMR administration (figure); rash onset occurred a median of 11 (range 7–18) days after MMR receipt. Most VARI (97%) occurred following first MMR dose. The presence of fever was similar among VARI and measles cases (97% of VARI vs. 100% of measles cases; P = 0.12), but differences were seen in the proportion with cough (30% vs. 96%; P < 0.001), coryza (47% vs. 85%; P < 0.001), conjunctivitis (23% vs. 68%; P < 0.001), and exposure to infectious measles cases (0% vs. 96%).
Conclusions
Surges in MMR administration and heightened community awareness during a measles outbreak can result in a large number of VARI, consuming considerable public health resources. When evaluating the need to suspect measles among patients with febrile rash, clinicians should consider time since MMR administration, clinical presentation, and history of measles exposure. Collecting appropriate specimens for timely virus genotyping could inform appropriate public health action.
Disclosures
All authors: No reported disclosures.
Articles from Open Forum Infectious Diseases are provided here courtesy of Oxford University Press
Source… https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5631265/